When I was in school going through my microbiology courses, it was hectic. Don't get me wrong, I loved those classes and my desire to do well was genuine. I remember setting up biochemical tests to identify organisms. I recall learning about different chemicals and memorizing the reaction patterns. Those classes taught me the old (I mean old) school way of testing.
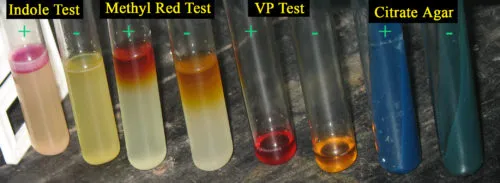
The classic set of reactions. There are dozens more depending on what you are testing.
I can't imagine where people got the idea of scientists having colored fluids from. /s
While playing with different colored tubes was fun, it was time consuming. Not to mention, the quantity of isolated bacteria needed to inoculate them. Then, the nightmare of keeping them organized and managing space ensued. Can you imagine doing that for the sheer number of patients a hospital encounters?
Lucky for us, the industry is far more advanced than that. I learned that firsthand when I visited a clinical laboratory.
One of the most useful tools for a microbiology lab are the BD BBL™ CHROMagar™ Orientation and TSA II I-Plate™. That's a mouthful, but we call it chrome agar for short. They are very useful for working through patient urine cultures.

It's a product photo you see.
The CHROM side of the agar provides a color indicator of presumptive identifications. The sheep blood side helps with colony types, morphology, and hemolysis. They complement each other. In terms of urine cultures, they also help determine if the specimen was a clean catch. In most urinary infections, there shouldn't be more than 1 or 2 organisms observed. The laboratory often dismiss cultures with 3 or more organisms as questionable. Although, clinicians are welcome to insist further testing.
In the stock image above, one could tell there are two different bacteria growing in the culture. They are most likely E. coli (pink) and a species of Enterococcus (blue). It's not uncommon for laboratory scientists to misread young blue colonies. This is where the blood side helps differentiate based on morphology.
You see how much easier that is when comparing to old school methods?
Then what?
As of now, the lab I work at uses the MicroScan WalkAway-96 Plus to process the high volume of cultures. That machine itself would take pages to explain, and we have five of them. The gist of it is that it does the biochemical, as well as the susceptibility, tests. The lab would evaluate the test results and then finalize them on the reports to clinicians.
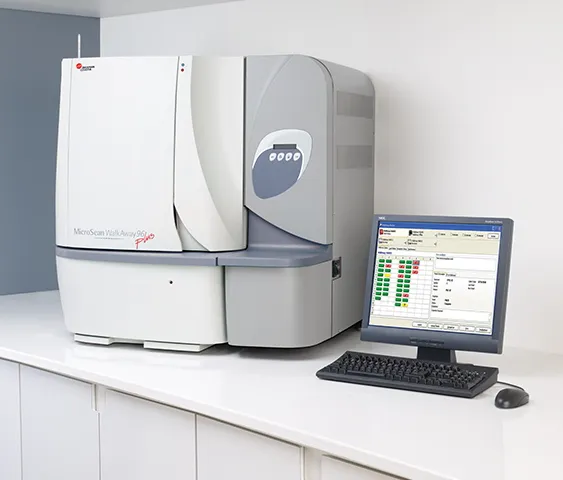
It's a beast and a chemical and water hog.
The clinicians can then treat their patients based on the data or request more testing as needed.
The tools of the trade help streamline an otherwise time-consuming and daunting process. In fact, there's a whole family of chrome agar that simplify testing altogether. Here's a pdf of some of the cool selective agar that I get to play with at work:
At least, the colors are pretty to look at. We have a saying in the lab that the cool stuff you see are usually the worst for the patients. I never cease to feel conflicted about seeing interesting test results. This is because I'm also reminded that the patients are most likely not having a good time.
Anyways, a quick summary involving the tools and processes mentioned above.
The Process
- Sample taken. Clinicians order tests and sent to lab.
- Go through lab processing. Cultures set up.
- Cultures read. Decide if cultures require tests. If not, skip to 6. If no growth, wait for another 18-24 hours.
- Results evaluated. Determine if they need more tests.
- Results finalized and sent to clinicians.
- The end. Unless clinicians want more tests or have questions.
The average turnaround time for urine cultures is between 35-42 hours. That's according to the last stat report I've seen from my supervisor. More complex cases could take longer. The lab goes through hundreds of them a day.