
New advances in cancer detection are offering a glimpse into the future of early diagnosis and personalized treatment, potentially transforming how the disease is identified and managed. A series of recent studies suggest that cancer may leave detectable traces in the blood long before symptoms appear or imaging can reveal a tumor. These findings are shaping hope that blood-based diagnostics—often called liquid biopsies—could catch cancer early, track its return, and guide therapy decisions more accurately than current methods.
One major breakthrough comes from a team at Johns Hopkins University, who found that cancer-related genetic mutations could be detected in blood samples up to three years before a diagnosis was made. Using blood specimens from a long-term cardiovascular study, researchers identified tumor DNA in several individuals who were later diagnosed with cancer. In some cases, these mutations were found more than three years before the patients experienced any clinical signs. This raises the possibility of intervening at a stage when the cancer is far less advanced and potentially more treatable.
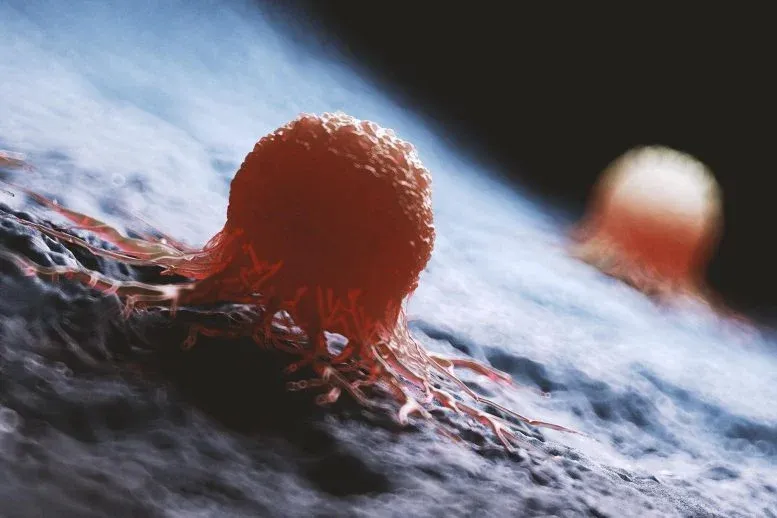
These tests look for circulating tumor DNA (ctDNA), tiny bits of genetic material shed by cancer cells into the bloodstream. By analyzing the DNA in blood samples, scientists can detect whether specific mutations linked to tumors are present. Early results are promising, but experts caution that much remains to be understood about how best to use these tests.
In clinical settings, particularly in patients who have already undergone cancer treatment, ctDNA tests offer a way to spot recurrence long before a tumor shows up on a scan. For instance, in a study from Yale published in Nature Medicine, ctDNA tests picked up signs of lung cancer relapse an average of five months before imaging did. This earlier warning could allow doctors to adjust treatment strategies—such as prolonging therapy or switching to a different medication—based on a patient’s real-time risk.
Yet with excitement comes caution. While the ability to detect cancer sooner is appealing, it's not yet clear if acting on this information improves patient outcomes. Some studies suggest that early detection of microscopic cancer cells correlates with a poor prognosis—patients whose cancer returns early, even at a molecular level, tend to fare worse. This raises difficult questions: Should doctors start treatment based solely on ctDNA results, even when no tumor is visible? Could they be exposing patients to the physical and emotional toll of additional therapies without clear benefit?
One encouraging study focused on colon cancer patients. After surgery, participants were either monitored using ctDNA analysis or received traditional care. Those who tested negative for tumor DNA were able to avoid chemotherapy, with no increase in cancer recurrence or death. This suggests ctDNA tests may help identify which patients actually need follow-up treatment and which could safely skip it.
Still, this is not the norm across all cancers. In breast and lung cancer, patients who tested positive for ctDNA after treatment were more likely to experience shorter survival times. Researchers are working to determine if earlier interventions in these cases could change those outcomes.
Another issue is cost. These personalized tests, which must be tailored to each patient’s tumor DNA profile, can run several thousand dollars. While they are currently offered in some clinical settings, many experts argue they should remain within research environments until more is known. The U.S. Food and Drug Administration has highlighted concerns about consistency across testing labs, and there’s still debate over how to handle positive results when no other evidence of disease is present.
In summary, ctDNA testing holds significant potential to change how cancer is detected and treated. The technology enables earlier detection and a personalized approach to monitoring, offering a powerful new tool in cancer care. However, its ability to improve survival—and not just generate more data—remains unproven. As researchers continue to study its applications, doctors and patients alike must weigh the potential benefits against the costs and uncertainties that come with this evolving form of surveillance.