Being already in the 5th year of my career, and my 2nd year of internships, things are not being as easy as I expected, but not for the reasons one would expect; as I said in the heading, the constant lack of the most basic public services is making all aspects of my life quite difficult. However, having previously downloaded several books helps, although I cannot find out about the most recent updates, and the lack of electricity leaves me with few things to do besides studying. It was during one of those nights, reading from my Tablet and writing my summaries literally by candlelight, that it occurred to me to study in another way, when the electric service would allow me to: write articles about the topics I needed to study, with my characteristic style. Nothing innovative, I know, but useful and entertaining, for me and I hope for you.
The first articles will deal with topics related to pediatrics, the area in which I am currently in, and one of my favorites; internal medicine on a small scale and with more challenges, basically. Focusing on today's article, I will talk about a relatively common syndrome that can easily be confused with other pathologies: the Nephritic syndrome.
Nephritic Syndrome in Pediatry
Kidney diseases can be easily confused among them; although the kidneys have a good number of different parts that can be affected independently, the symptoms are often similar, and the diagnosis is almost always based on laboratory tests. Perhaps this is why one of my role models (more in terms of preparation and knowledge than in the treatment of patients), Dr. Gregory House, is a nephrologist; with the character a kind of Sherlock Holmes with a medical degree, it is to be expected that his specialization is one in which the final diagnosis is often a difficult-to-decipher mystery.
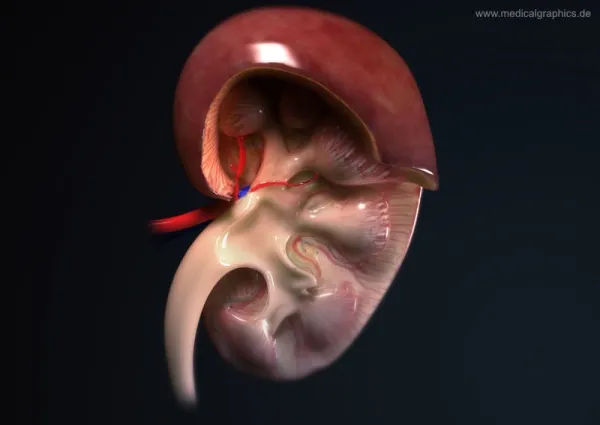
One of these diseases is the Nephritic Syndrome, a condition that, although has a set of specific symptoms which I will explain later, may have a difficult cause to pinpoint. This syndrome is defined as a defect in the glomerulus, which is basically a cluster of capillaries (small arteries) surrounded by an outer semicircular envelope called the Bowman's Capsule, which is found in the nephrons (basic functional unit of the kidneys). It is in the glomerulus where the purification and filtration of the blood occurs, and the first stages of the process of urine formation based on the substances that are eliminated. The glomerulus, together with Bowman's capsule, constitute the so-called Renal Corpuscle, which is the basic filtration unit of the kidneys.
The nephritic syndrome usually has an acute onset, and is characterized by the triad of hematuria (blood in the urine), edema (swelling caused by fluid accumulation), and high blood pressure, although it is usually accompanied by other symptoms, usually caused by inflammation of the glomeruli. However, it is important to bear in mind that this syndrome does not always occur in a complete form, so to speak, and in fact, the term "nephritic syndrome" is currently falling into disuse in some countries, being replaced by the underlying pathology causing the symptoms suffered by the patient, such as glomerulonephritis (inflammation of the glomeruli commonly caused by bacterial infections), or by systemic autoimmune diseases such as Systemic Lupus Erythematosus. That is why the terms of nephritic syndrome and acute glomerulonephritis are often used interchangeably, although it is true that the nephritic syndrome may have other etiologies, and may not always present the same symptoms, since, ultimately, they are two different diseases.
This syndrome is the most common kidney disease in children, especially in those of school age with predominance between 6 and 7 years, and is usually associated with glomerular nephropathies. The most common cause is an acute post-streptococcal glomerulonephritis, that is, due to an infection by streptococcal bacteria, usually by group A beta-haemolytic streptococcus that produces an infection in the pharynx or skin, which then affects the glomerulus. The second most common cause is an autoimmune disease known as IgA Nephropathy (by immunoglobulin A) in which an anomalous accumulation of the antibody immunoglobulin A in the glomeruli causes an inflammation, and the third most common cause is Systemic Lupus Erythematosus, another autoimmune disease. In addition to beta-hemolytic streptococcus, other agents have been associated with acute glomerulonephritis, such as Staphylococcus aureus, mycobacteria, Epstein-Barr virus, cytomegalovirus, and parasites such as Plasmodium, Toxoplasma gondii and Trypanosomes.
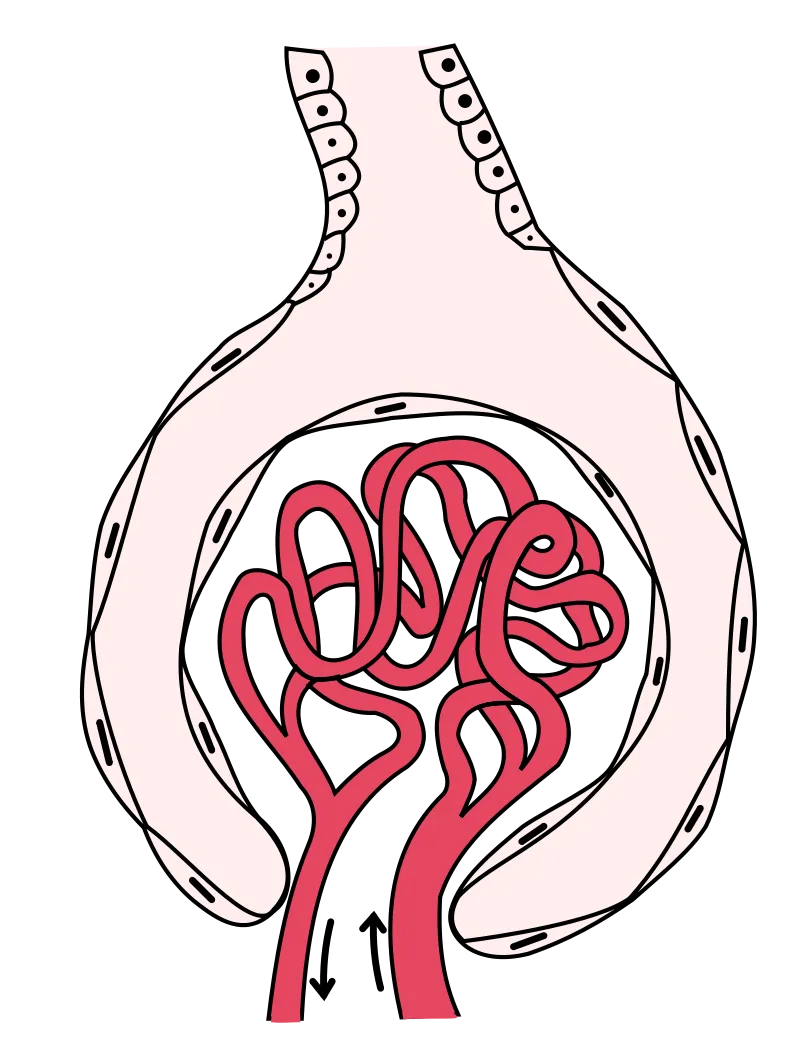
Drawing of a glomerulus, inside the Bowman Capsule.
Regarding the physiopathology, the most common element in the nephritic syndrome, as I said previously, are lesions in the glomerulus, caused by an infiltration of immune cells, mainly leukocytes (white blood cells). This causes an inflammatory reaction that damages the walls of the glomerular capillaries, allowing erythrocytes and red blood cells (main components of the blood) to escape into the urine, causing several hemodynamic alterations that decrease the filtering rate in the glomeruli, causing oliguria (decrease in daily urine volume), because less urine is produced due to problems with blood filtration, and causing a system called Renin-Angiotensin-Aldosterone to activate, producing an increase in the blood pressure. In addition to this, there is an increase in the permeability of the glomeruli, causing the red blood cells and the proteins found in the blood to go out in the urine, and to increase the urea and creatinine, toxic substances normally expelled through urine, which are then reabsorbed into the bloodstream.
Among its symptoms we have already highlighted hematuria, the most common clinical finding and that in more than half of cases is usually visible to the naked eye. When the syndrome is caused by a bacterial infection, the hematuria appears 1 or 2 weeks after an infectious process in the pharynx or tonsils, and 3 to 4 weeks after a skin infection. There is also arterial hypertension, a consequence of the retention of fluids and sodium and the secretion of renin by the kidneys, edema mainly localized in the face, eyelids and extremities and that occurs predominantly in the morning, proteinuria (presence of proteins, such as albumin, in urine), oliguria due to fluid retention, and in severe cases it may cause renal failure.

Classic example of edema caused by nephritic syndrome
For its diagnosis it is important to inquire about the existence of previous infections or autoimmune diseases such as lupus, and the family medical history should be investigated in search of a history of nephropathy or consumption of drugs or medicines that may have damaged the kidneys. In addition to this, it is important to ask about the appearance and color of the urine. In the physical examination the presence of edema, blood pressure, and signs that may indicate the existence of renal failure must be assessed, just as the pharynx should be examined for signs of previous infections. The laboratory tests are of great importance in order to reach a concise diagnosis, the main one to be performed is the analysis of urine where red blood cells and proteins will be present in generally moderate amounts, and if there is a massive proteinuria, can lead us to think that the etiology is an autoimmune disease. The blood electrolyte and biochemistry studies are also essential; sodium will be low, as will albumin and proteins, while urea, creatinine, and urea nitrogen will be elevated. Finally, the imaging studies can also be useful, such as a renal ultrasound in which the kidneys will be inflamed and hyperechoic.
It is necessary to make a differential diagnosis between the nephritic and nephrotic syndrome, due to the similarity between some of its clinical manifestations. The nephritic syndrome produces a decrease in glomerular patency, has a higher incidence between 5 and 15 years of age, usually occurs after a cutaneous or pharyngeal infection and with a sudden onset, and its clinical manifestations, such as mild to moderate hematuria and proteinuria, hypertension, and mild edema, are related to the decrease in glomerular filtration rate, fluid retention, and the increase of nitrogen compounds in the blood. The nephrotic syndrome, on the other hand, causes an increase in glomerular patency, it is more common in children under 5 years of age, its onset is progressive and there is usually no history of previous infections. The clinical manifestations are different; there is only proteinuria (without hematuria) which is usually massive, there is no arterial hypertension, the edema is severe and can spread to the abdomen (anasarca), there is hyperlipidemia (increase in lipids in the body), and its symptoms are related to the large loss of plasma protein.
There is no specific treatment for the nephritic syndrome, the measures to be taken are symptomatic and supportive, aimed mainly atsolving hypertension and edema. Glomerulonephritis, which is the most common etiology, is usually temporary and reversible, although it can sometimes worsen and cause chronic renal failure. At ambulatory level absolute rest should be recommended for 3 to 5 days as well as a diet low in sodium and protein, in addition to limiting water intake; this if the syndrome and its symptoms are mild. If, on the other hand, the patient has significant edema, severe hypertension, a significant decrease in urinary output and/or severe haematuria, it must be hospitalized. In addition to rest and diet, a pharmacological treatment should be started, using diuretics such as furosemide, hydralazine and nifedipine for high blood pressure, and in forms of rapid progression, corticosteroids such as dexamethasone can be used to decrease the glomerular inflammation. If its etiology is infectious, antibiotics such as penicillin are used to eliminate the causative agents, and in severe cases, or if there are important electrolyte alterations, dialysis should be indicated.
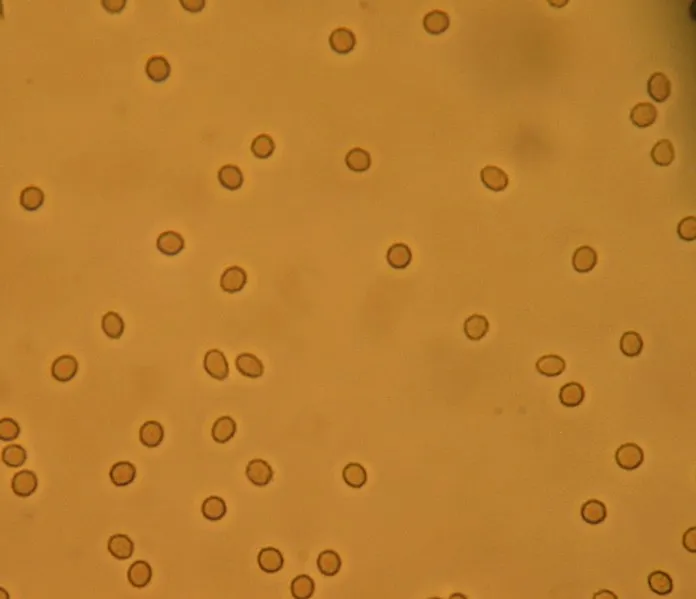
Microscopic view of the hematuria.
Finding urine in the blood can be a dramatic occurrence, and understandably, it can be thought to be due to a serious illness with lasting consequences, but as we can see, this is not always the case. The nephritic syndrome, in most cases, does not endanger the life of the patient and its symptoms are relatively mild compared to the nephrotic syndrome, about which I will speak in a future article. With this, we can realize that in medicine, the severity of the disease is not always related to the symptoms (except in the area of surgery, injuries and injuries are usually as serious as they appear), so you do not always have to be frightened when presenting some apparently serious sign or symptom; it may be something that does not even require treatment.
References:
- Nephritic Syndrome – An Overview
- Nephritic Syndrome – Pediatrics in Review
- Pediatric Nephritis – Medscape