
How do you stop the world’s most effective killing machines?
Mosquitoes spread disease on a terrifying scale. Annually, mosquito-borne diseases are responsible for the loss of approximately 100 million years’ worth of healthy life (i.e. 100,000,000 DALYs per year, (see previous post for an explanation of this concept) and they are responsible for the vast majority of the transmission, suffering and deaths caused by the following diseases and many more:
Data is from here, here and here.
With these little bastards causing more suffering in the world than any other insect or animal (yes that includes us humans, well sort of) I was excited to hear, this week, of a new intervention for their control that may very soon be brought into play.
Mosquitoes as a vector of transmission
In epidemiology, a vector is any agent that is responsible for transmitting a pathogen to another organism 1. For the above diseases their main vector for transmission is the mosquito. Mosquitos don’t contract the diseases themselves in this case, but instead carry diseases from one human to another as they go about their day to day business of sucking tasty blood out of unsuspecting, soon-to-be-pissed off and itchy mammals.
This presents an interesting opportunity for those of us who work in global health. Instead of treating the diseases when patients start to show symptoms, or vaccinating for the diseases one at a time, we can find a means of cutting the diseases off at their shared vector and as such reduce the prevalence of all mosquito-borne diseases at once.
With mosquito-borne diseases, there are a number of vector control methods available in our toolkit. Spraying houses with insecticides 2, removing standing water, genetically engineering mosquitoes to make them sterile 3, and even the use of Guppies 4 (this is one of my friends’ wonderfully strange, but effective, areas of research) all have their place in vector control. However, currently the most effective vector control method, by a long way, is bed nets.
Bed nets are perfect for this job, as the mosquitos that commonly carry the diseases in question mostly come out at night (mostly). As such, sleeping under a physical barrier such as a fine mesh mosquito net prevents the mosquitoes from getting anywhere near the individual underneath. If the net is well made, undamaged and used correctly, this intervention is 100% effective.
But that doesn't mean 100% is the most effective that this intervention can be. No, no, no, we can in fact do far better than this!
Long lasting insecticide treated bed nets
Long-lasting insecticide treated bed nets (LLINs or ITNs) are one of the most spectacular innovations to come out of evidence-based global health in a long time (they’re no PlayPumps, that's for sure).
Not only do these special nets offer a durable physical barrier against mosquitos, but they are coated with an insecticide designed to kill any mosquito that lands on it (when a mosquito is killed in this way it’s known as knock down, how lovely a phrase is that?). This not only means that us tasty humans under the nets are protected by a lightweight breathable barrier, but also, occasionally, that barrier takes a disease-carrying mosquito out of the sky for good, ensuring that they don’t infect anyone else. As such, the nets are able to provide a small community benefit as well 5, similar to that of herd immunity found with vaccines.
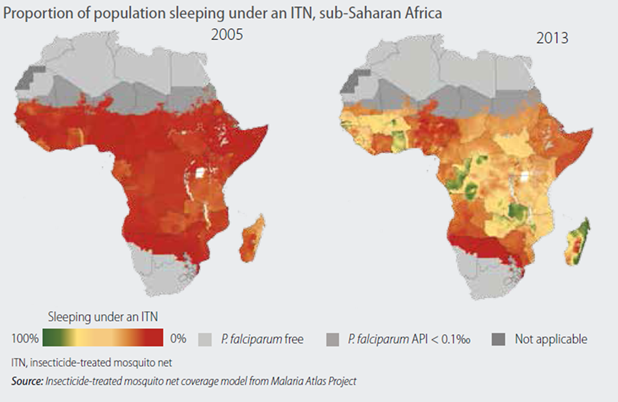
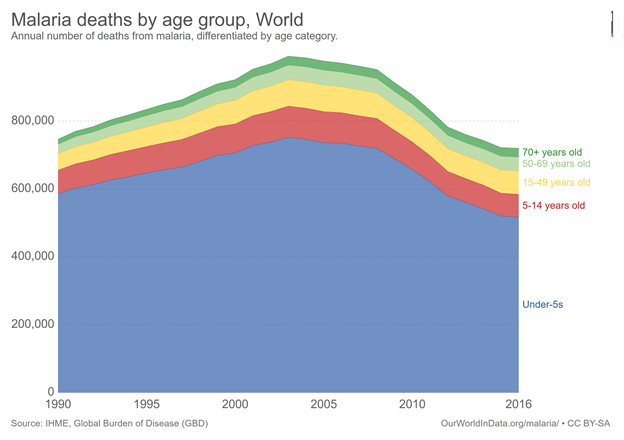
Since their development, the roll-out of these nets has been extensive. It is now estimated that 54% of African households at risk of malaria now sleep under LLINs. Since 2000, malaria cases and deaths have reduced by 60%, with the LLINs often being credited with an amazing 70% of this reduction. They are very good nets!
The effectiveness of the current LLINs all comes from the pyrethroid insecticides they are treated with. Harmless to humans, this insecticide kills some, but not all, of the mosquitoes that land on the nets. The ones that the insecticide doesn’t kill likely have a natural immunity to the insecticide. The killing of those that don’t have immunity, and the survival and reproduction of those that do, sadly causes resistance to the insecticide to be selected for.
This leaves us with a problem. The more we use the nets (and spray houses with the insecticide) the quicker the mosquitoes adapt to the insecticide and the less effective it becomes. Using these nets therefore may mean a reduction in disease in the short term but an inevitable bounce back as the mosquitoes evolve to be resistant to the insecticide. This had lead many who work in global health to be concerned about the future of malaria control programs 6.
Although now there is a promising development on the horizon.
Try our new and improved LLINs now with added Piperonyl Butoxide!
The chemical Piperonyl Butoxide (PBO) is what is known as a synergist; a chemical that makes insecticides more effective. PBO acts to inhibit crucial enzymes in the natural defense mechanisms of the mosquitoes, effectively removing their resistance to the insecticide coating the nets and rendering it deadly again.
A nifty solution, eh? The mosquito evolved a defense and we developed a way to turn off that defense.
So according to the science this could be a highly useful tool in our mosquito vector control toolkit. As for the field evidence, initial findings look promising, with a recent double-blinded (yes you can actually double-blind with this intervention) cluster RCT demonstrating a significantly lower malaria prevalence after 9 months of use in the PBO insecticide treated nets compared to the LLIN nets 7.
This was from a relatively small trial of N=7,184 so now it’s time to scale up and test the nets further. Over the last year or so The Against Malaria Foundation have funded the distribution of 6 million POB nets to areas with particularly high levels of insecticide-resistant mosquitoes in Uganda. They, again, intend to compare the health outcomes of these 6 million users to a control group using the standard LLINs.
In a statement released this week The Against Malaria Foundation say:
”By understanding to what extent PBO nets can play a role in combating insecticide resistance in mosquitoes, the ultimate value of this study is to help net funders, including health ministries, make informed decisions about the nets they purchase and distribute that will optimize malaria control.”
Results from this study will likely be published in the spring of 2019 and if the results warrant it this could see a substantial shift in how we control mosquitoes on a global scale.
About me:
My name is Richard, I blog under the name of @nonzerosum. I’m a PhD student at the London School of Hygiene and Tropical Medicine. I write mostly on Global Health, Effective Altruism and The Psychology of Vaccine Hesitancy. If you’d like to read more on these topics in the future follow me here on steemit or on twitter @RichClarkePsy.
Also I’m in the process of building up my Steem basic income shares so I’ve decide to sponsor a share a week to someone that engages in the comments below. I’ve no real system for this but get stuck in and I'll likely sponsor you in at some point.
References:
[1] The World Health Organisation: Vector borne diseases
[2] The World Health Organisation: Core vector control methods
[3] Harris AF, Nimmo D, McKemey AR, Kelly N, Scaife S, Donnelly CA, Beech C, Petrie WD, Alphey L. Field performance of engineered male mosquitoes. Nature biotechnology. 2011 Nov;29(11):1034.
[4] Hustedt J, Doum D, Keo V, Ly S, Sam B, Chan V, Alexander N, Bradley J, Prasetyo DB, Rachmat A, Muhammad S. Determining the efficacy of guppies and pyriproxyfen (Sumilarv® 2MR) combined with community engagement on dengue vectors in Cambodia: study protocol for a randomized controlled trial. Trials. 2017 Dec;18(1):367.
[5] Levitz L, Janko M, Mwandagalirwa K, Thwai KL, Likwela JL, Tshefu AK, Emch M, Meshnick SR. Effect of individual and community-level bed net usage on malaria prevalence among under-fives in the Democratic Republic of Congo. Malaria journal. 2018 Dec;17(1):39.
[6] Hemingway J, Ranson H, Magill A, Kolaczinski J, Fornadel C, Gimnig J, Coetzee M, Simard F, Roch DK, Hinzoumbe CK, Pickett J. Averting a malaria disaster: will insecticide resistance derail malaria control?. The Lancet. 2016 Apr 23;387(10029):1785-8.
[7] Protopopoff N, Mosha JF, Lukole E, Charlwood JD, Wright A, Mwalimu CD, Manjurano A, Mosha FW, Kisinza W, Kleinschmidt I, Rowland M. Effectiveness of a long-lasting piperonyl butoxide-treated insecticidal net and indoor residual spray interventions, separately and together, against malaria transmitted by pyrethroid-resistant mosquitoes: a cluster, randomised controlled, two-by-two factorial design trial. The Lancet. 2018 Apr 21;391(10130):1577-88.
Additional sources:
Alfaro-Murillo JA, Parpia AS, Fitzpatrick MC, Tamagnan JA, Medlock J, Ndeffo-Mbah ML, Fish D, Ávila-Agüero ML, Marín R, Ko AI, Galvani AP. A cost-effectiveness tool for informing policies on Zika virus control. PLoS neglected tropical diseases. 2016 May 20;10(5):e0004743.
